Nasal Bone
First Trimester Examination of the Fetal Nasal Bone
The findings of recent studies suggest that examination of the fetal profile at 11-13+6 weeks could have major beneficial implications in screening for Trisomy 21 by maternal age and fetal nuchal translucency (NT). However it is imperative that, as for the NT scan, sonographers undertaking risk assessment by examination of the fetal profile must receive appropriate training and certification of their competence in performing the nasal bone scan.
This document describes the Fetal Medicine Foundation:
- Protocol for the assessment of fetal nasal bone
- Clinical application of nasal bone findings
- Certification in the first trimester assessment of the fetal nasal bone
Protocol for the assessment of fetal nasal bone
- The gestational period must be 11 to 13+6 weeks - the nasal bones first appear at a crown-rump length of 42 mm and increase linearly with gestation
- The magnification of the fetus must be such that only the head and upper thorax are present on the screen
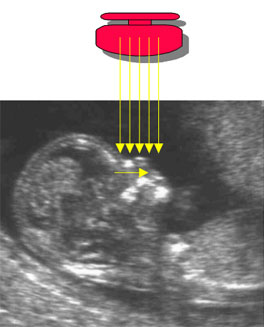
- A mid sagittal section of the fetal profile must be obtained with the ultrasound transducer held parallel to the direction of the nose. The ultrasound transducer should be gently tilted from side to side to ensure that the nasal bone is seen separate from the nasal skin
- The echogenicity of the nasal bone should be greater that the skin overlying it. In this respect, the correct view of the nasal bone should demonstrate three distinct lines:
- The first two lines, which are proximal to the forehead, are horizontal and parallel to each other, resembling an “equal sign”. The top line represents the skin and bottom one, which is thicker and more echogenic than the overlying skin, represents the nasal bone
- A third line, almost in continuity with the skin, but at a higher level, represents the tip of the nose
Absence of the bottom line of the equals sign represents the absence of the nasal bone.
When the nasal bone line appears as a thin line, less echogenic than the overlying skin, it suggests that the nasal bone is not yet ossified, and it is therefore classified as being absent.
Clinical application of nasal bone findings
The incidence of an absent nasal bone is related to NT, CRL and ethnic origin as well as aneuploidy, being more common with increased NT, smaller CRL measurements and in fetuses of Afro-Caribbean parents. Therefore it is not possible to give simple numbers by which the presence of the nasal bone will reduce the risk for Trisomy 21 and the absence will increase the risk. The Fetal Medicine Foundation software includes the nasal bone in the calculation f risks but access it available only to sonographers who have been appropriately trained and accredited in the assessment of the fetal nasal bone.
The software firstly calculates a risk based on maternal age, fetal nuchal translucency and maternal serum free beta-hCG and PAPP-A. If the risk is more than 1 in 50 and the nasal bone is present then the risk does not change. If the risk is 1 in 50 to 1 in 1,000 and the nasal bone is present the risk is usually reduced. If the nasal bone is absent the risk is always increased. The difficulty is in a patient with a low risk result from NT (with or without serum biochemistry) when the nasal bone appears to be absent. In this cases our advice is that the patients are rescanned in one week and action is only taken at that point if there is persistence of the absence of the nasal bone.